Malaria
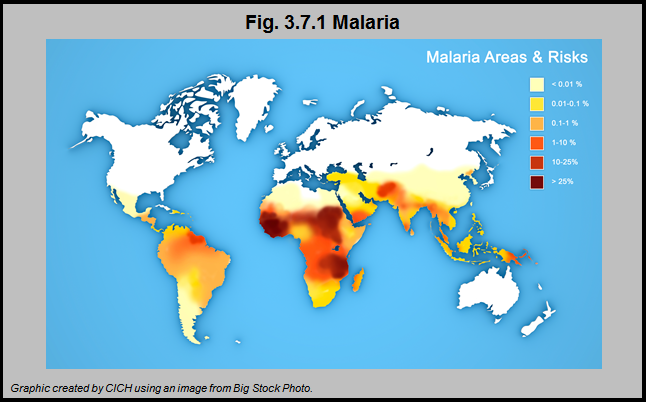
Malaria causes hundreds of millions of infections and an estimated one million deaths per year worldwide, many of which occur in children. Sub-Saharan Africa bears a significant proportion of the worldwide burden of malaria. The intensity and seasonality of malaria transmission varies significantly both within and among countries in the region and thus risk of malaria will vary between geographical locations, the age and ethnicity of the child and the time of year.
The symptoms of malaria (malaise, myalgia, headache and fever) are not exclusive to malaria and thus primary care practitioners may not readily recognize them as symptoms of malaria. Delays in the diagnosis and treatment of P. falciparum infection (the most dangerous type of malaria) may lead to severe disease and even death. Migrants who have lived or travelled in malaria-endemic areas are vulnerable to acute malaria, particularly within the first three months after arrival in Canada.
Implications
Routine screening of immigrant children and youth (and adults) for malaria is not recommended in the Canadian Immigrant Health Guidelines, but clinicians should be vigilant for symptoms of malaria – particularly when caring for children who have lived or traveled in malaria-endemic regions within the previous three months – particularly if they have fever. They should perform timely diagnostic inquiry and testing.1
Improved surveillance for malaria is needed in Canada, as well as more research related to the utility of screening immigrants and refugees for this disease.
For the Canadian Immigrant Health Guidelines click here.
1Pottie K, Greenaway C, Feightner J, et al. Evidence-based clinical guidelines for immigrants and refugees. CMAJ 2011;183:E824-925
